Cardiac Transplants
What happens when the heart stops working properly? In some cases, a heart transplant is one solution to restore life. When thinking of the human body as a computer, the brain is the hard drive—the processor where everything is stored, and signals are sent to execute and dictate responses. The heart is the power supply—without it, nothing works, and no systems turn on. The heart sends electrical pulses, making its chambers expand and contract in a specific order, creating a heartbeat. These pulses supply energy to every system in the body, allowing it to function properly. In addition to the pulses, the heart also pumps blood to all body parts, supplying the specific oxygen and nutrients needed to perform its purpose. Due to these functions, if the power is turned off, then everything starts to shut down, as organs need a constant supply of blood oxygen (Minnesota Medical Training Services, 2016).
A heart transplantation can be a life-changing procedure, however, due to a heart donor shortage the procedure is uncommon with approximately 5,000 surgeries taking place a year. A heart transplant is an operation where the diseased and failing heart is replaced with a healthier one from an organ donor. Patients can live for decades with various types of low-grade heart failure because heart transplants are only performed in the end stage of heart failure. If a patient is diagnosed with heart failure, it means their heart muscle cannot keep up with its workload of pumping blood sufficiently throughout the body because it is severely damaged or weak, which poses the threat of the body not receiving enough oxygen. A heart transplant is performed when other treatments such as medications, procedures, and surgeries for heart problems have not improved the condition (Johns Hopkins, 2019).
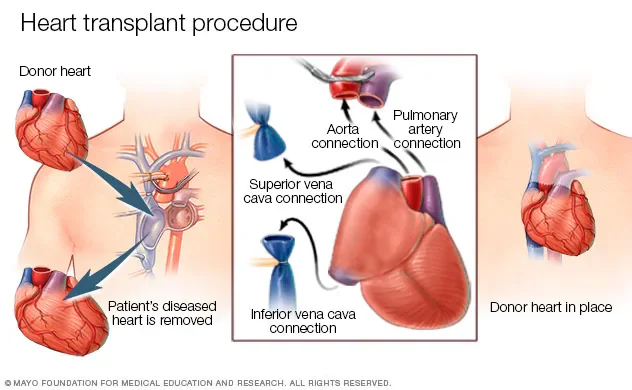
There are two different surgical procedures for heart transplants: orthotopic and heterotopic. An orthotopic heart transplant is much more common, where the recipient's heart is replaced with the donor heart. If a patient consents to donating their organs once declared brain dead, their heart must be removed, properly preserved, transported, and transplanted into the recipient within four to five hours. Hearts are offered first to a nearby transplant center and then to centers within certain distances of the donor hospital. Once the surgery has begun, the patient receives general anesthesia, putting them into deep sleep. Once sedated under general anesthesia, the patient is connected to a ventilator by inserting a tube down their throat which keeps the patient breathing during the surgery. The patient is then connected to a cardiopulmonary bypass machine, which takes on the role of the heart and lungs during the transplant surgery so the patient can be kept alive without a heart in the body. The machine adds oxygen to the patient's blood and removes carbon dioxide while maintaining blood circulation to all other organs and tissues. The surgeon adds blood thinners to the patient’s blood reducing the risk of blood clots when the blood flows through the heart-lung bypass machine. Blood clots are dangerous because they can block organs, posing the threat of shutting them down. Surgeons will then make an incision in the chest, separating the chest bone, and opening the rib cage so they can operate on the heart. Blood vessels connected to the heart are clamped down to disconnect them from the heart. When the donor’s heart has arrived, the recipient is prepared to avoid losing precious time with the donor's heart. The surgeon removes the diseased heart, then the donor heart is ready to fit and implantation begins. The donor's heart is sewn into place, and the major blood vessels are attached to the donor's heart. The surgeons begin warming up and restarting the new heart. Often, the new heart begins beating once blood flow is restored. However, an electric shock by a defibrillator device, which applies an electric charge to the heart may be needed to help the heart start beating properly (United Network for Organ Sharing, 2003).
The other surgical technique, the heterotopic heart transplant (also called "piggyback" transplantation), involves leaving the recipient’s heart in place while the surgeon connects the donor heart to the right side of the patient's chest. This procedure is rare because it is challenging to connect two hearts effectively, managing two hearts poses issues with blood flow regulation and rejection, specific indications, and because of the overall shortage of donor hearts. However, it is beneficial because the new heart can act as an assist device if complications occur through being attached in a parallel frame (United Network for Organ Sharing, 2003).
While there are multiple risks of complications both during and after the procedure, a combination of technology and anti-rejection drugs has significantly improved survival rates since the late 1900s. During the procedure itself, some risks include bleeding, infection, and blood clots. When the surgery is finalized, patients are transferred to the Cardiothoracic Intensive Care Unit for close monitoring in case early post-surgical complications arise. One of the biggest risks after the procedure is the body’s rejection of the donor's heart. This occurs because the immune system rightfully detects the heart as a foreign object and tries to attack or reject it, damaging the heart. Accordingly, right after the transplantation procedure and for the rest of their lives, the patient receives necessary medications to prevent rejection, which are called immunosuppressants. To detect rejection, the patient will undergo regular heart biopsies after the transplant. These biopsies are where a small amount of tissue from the inner lining of the heart muscle is removed and a pathologist examines the tissue under a microscope for any abnormalities. During the first year post-op, biopsies are frequent as it is a critical year when physicians must find the correct immunosuppressive medications that work for each individual patient. However, immunosuppressants have adverse effects as all medications have, including serious kidney damage, cancer, and infections because they decrease the body’s capability to fight off malignant cells and infections. This is one of the complications physicians are aware of and monitor closely in every case after transplant. Even though the immune system may not reject the donor heart, the donor heart may not function properly. This is the most frequent cause of death after the first few months or years after transplantation. After transplantation, the patient’s walls of the arteries in the heart can thicken, harden, and narrow, which leads to cardiac allograft vasculopathy. This limits blood circulation to the heart, and when severe, may cause a heart attack, heart failure, heart arrhythmias, or sudden cardiac death. Another common cause of death after the procedure is called primary graft failure where even a well-matched donor heart does not function best during the first few months, however, this is monitored closely as well (Cleveland Clinic, 2023).
For individuals who cannot become a heart transplant candidate or for those who are candidates but cannot find a matching heart, an alternative may be a ventricular assist device (VAD). It is a mechanical pump implanted in the chest, connected to the heart, that helps pump blood from the lower chambers of the heart, called ventricles, to the rest of the body. The VADs were originally designed as temporary treatments for patients waiting for heart transplants, but as there is a shortage of cardiac donors they are now indicated as definite therapies, meaning that these patients will never become transplant candidates. However, if a VAD does not help the patient's heart and serve its purpose, doctors may consider a total artificial heart, which is another type of device that replaces the ventricles of the heart and gains control over the pumping function. This may serve as an alternative short-term treatment while waiting for a heart transplant (Mayo Clinic, 2019).
Organ transplantation is one of the most significant advances in modern medicine. Heart transplants allow an individual to stay alive who without it, would have life-threatening diseases and injuries. Heart transplantation may significantly improve the quality of life for patients, as many end stage heart failure patients are either living in hospitals connected to multiple therapies or are deemed for palliative treatment which implies allowing the patient to pass.
References
Cleveland Clinic. (2023, October 11). Organ donation & transplantation. Retrieved October 27, 2024, from Cleveland Clinic website: https://my.clevelandclinic.org/health/treatments/11750-organ-donation-and-transplantation
United Network for Organ Sharing (UNOS). (2003, August 1). Heart - How does your heart work? Retrieved October 27, 2024, from UNOS Transplant Living website: https://transplantliving.org/organ-facts/heart/
John Hopkins Medicine. (2019). Heart Transplant. Retrieved October 27, 2024, from Johns Hopkins Medicine website: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/heart-transplant
Mayo Clinic Staff. (2019). Heart transplant - Mayo Clinic. Retrieved October 27, 2024, from Mayoclinic.org website: https://www.mayoclinic.org/tests-procedures/heart-transplant/about/pac-20384750
Minnesota Medical Training Services. (2016, August 16). Why Exactly is the Heart So Important? Retrieved October 27, 2024, from Minnesota Medical Training Services website: https://www.minnesotacpr.com/exactly-heart-important/